We are thrilled to have the opportunity to feature the father-daughter duo, Doug and Annie Ritter, on our website. Both Doug and Annie have dedicated their lives to the medical field and share a passion for improving healthcare worldwide. Doug is a retired orthopedic surgeon who recently graduated with a Graduate Certificate in Global Surgical Care (GCGSC), while Annie is a highly accomplished general surgeon who is currently in a trauma fellowship with the University of Calgary and began the Master of Global Surgical Care (MGSC) this year. With their combined knowledge and expertise, they have made a significant impact on the medical community and those in need of quality surgical care in low resource settings, particularly in Bhutan. We are honored to share their stories and experiences with our readers.
 Dr. Doug Ritter is a semi-retired orthopedic surgeon currently working in Kemptville, Ontario and previously at the Queensway Carleton Hospital in Ottawa, Ontario. He graduated with the Graduate Certificate in Global Surgical Care in May 2022.
Dr. Doug Ritter is a semi-retired orthopedic surgeon currently working in Kemptville, Ontario and previously at the Queensway Carleton Hospital in Ottawa, Ontario. He graduated with the Graduate Certificate in Global Surgical Care in May 2022.
Dr. Annie Ritter is a highly accomplished general surgeon in trauma fellowship with the University of Calgary. She holds a Bachelor of Medicine, Bachelor in the Art of Obstetrics and Bachelor of Surgery (MB BAO BCh). Her passion for global surgical care has lead her to do a volunteer observership in Bhutan with her father Doug. Annie’s dedication to helping those in need is a testament to the Ritter family’s commitment to improving global healthcare. Her expertise in trauma surgery and education background make her a valuable asset to the healthcare industry. Following in her father’s footsteps, Annie enrolled in the Master of Global Surgical Care in September 2022.
Read on to find out more about Doug and Annie, their background and experiences, what lead them to the GCGSC and MGSC programs, and more!
What has inspired you to study and work in the field of global surgery?
Doug: I had the opportunity to live in Europe and travel frequently with my family at a young age, so the travel bug began early. During medical school, I visited my father in Nairobi, Kenya, who was working for the Canadian International Development Agency (CIDA) at the time. We toured a local hospital which definitely piqued my interest. The idea of volunteering and working outside the country continued to be an interest following medical school. I chose to specialize in orthopedics after doing emergency medicine, knowing that orthopedics was essential throughout the world. However, after finishing orthopedics training, with a young family and building an orthopedic practice, it was very difficult to consider volunteering. Opportunities did not seem easily available at that time.
Later through colleagues, I discovered Health Volunteers Overseas (HVO) and I volunteered with them, initially in St. Lucia and subsequently in Bhutan. Volunteering in St. Lucia was simpler and only required a two-week commitment to allow the local surgeon to take a holiday. In Bhutan, there was a great need for orthopedic care with two surgeons for 800,000 people and very limited resources. The volunteer requirement is now a minimum of five weeks. Travel, adventure, the overwhelming need, and personal development and education were driving factors in volunteering.
Annie: My father!

What are some of your hobbies & interests? What do you love to do in your spare time?
Doug: Our entire family would play squash in the past. We also ski (with our grandchildren too!), play chess and travel. During the summer months, we often visited our cottage and enjoyed outdoor activities and also exploring new destinations and experiences.
Annie: Squash, snowboarding, travel, walking my dog.
What advice would you give to someone just starting out in global surgery and to prospective students?
Doug: Commit yourself as soon as possible. Start with shorter time frames, which are much easier to arrange. There is some advantage in returning to the same place as you know the ropes and don’t spend half your time learning what to do. I believe your time is much more efficient that way. I have chosen locations that are safe for family and also as an individual. If you have children, they can often attend a local school. Your partner or other family members may find there are many other ways to volunteer with groups or teams. I have no experience in that, however, as I was always on my own. With HVO, the main purpose was teaching rather than providing large amounts of “service”. At that time, there were no courses to take to guide me when I started volunteering. HVO was helpful in preparing the way and giving advice. Now even a preliminary class in global medicine or surgery could make the entire volunteer experience more useful for everyone involved, such as what is offered in the GCGSC.
Annie: You don’t have to be a surgeon to get involved! Any allied health professional could take these programs.


We are fascinated with your experience of volunteering in Bhutan, can you tell us a bit more about it? What do you do there and what sparked your interest in volunteering?
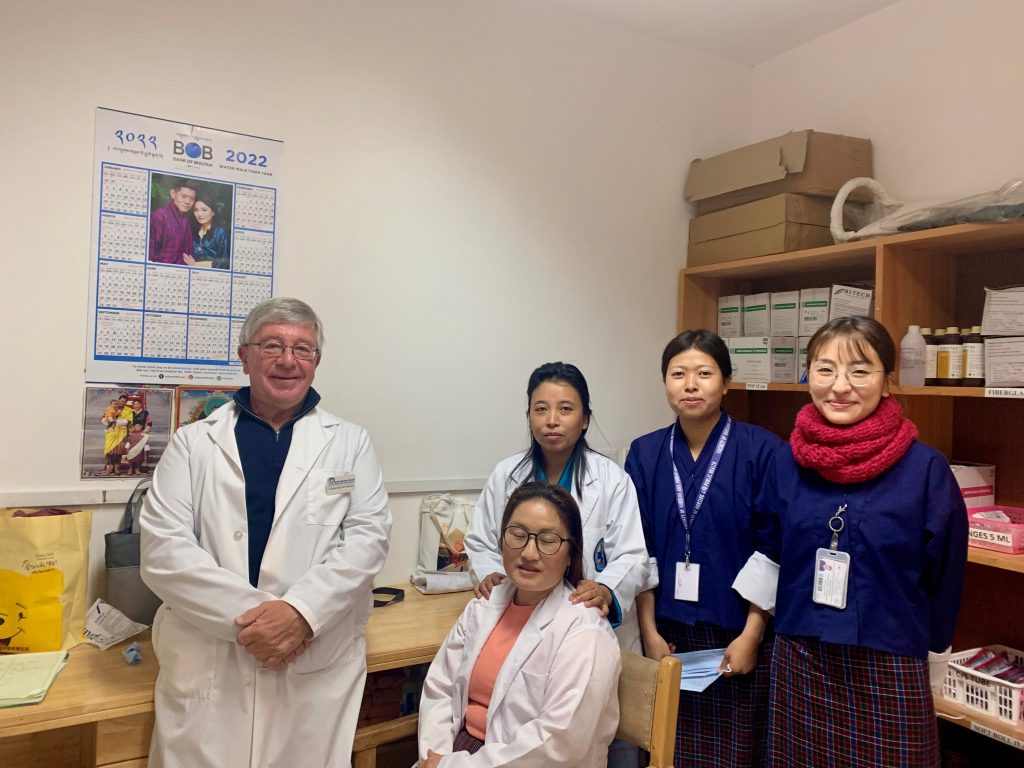
Doug: A program to teach orthopedic technicians, or orthopedic physician assistants, due to a severe lack of human resources in the country, had been developed by volunteers and local surgeons in the early 2000s. One of my main tasks was to teach each morning for one hour, a specific aspect of orthopedics, such as knee examination and pathology, treatment of osteomyelitis or club foot treatment.
The course was extensive covering all aspects of orthopedics for young high school graduates. I was one of many volunteers teaching from 2003 until 2016. Each month, a different orthopedic volunteer would come to teach a specific part of the orthopedic course. It was a very popular volunteer experience. Many volunteers brought their families.
The other parts of the job were to see patients in the clinic at the same time and teach the orthopedic assistants. Assisting and sharing orthopedic techniques with the local surgeons in the operating room was also a significant part of the job.
I always had the feeling that I was learning more from local surgeons than I was teaching in these circumstances. They were very adept at using minimal resources. The fact that I had trained in the 1970s actually was beneficial to me as many low-resource surgical techniques were familiar to me.
As Bhutan’s medical training advanced, I became involved in teaching interns in 2013 and 2016.
They now have a post-graduate orthopedic program and much of my time is spent with five orthopedic residents. Every morning there are teaching rounds and every day is clinic day, so there is ample opportunity for orthopedic teaching. Patient care is ongoing every day.
Local surgeons have risen to the occasion and are excellent teachers for their resident staff. When I started in 2003 there were 2 Bhutanese surgeons. This gradually increased over the years and there are now five in the main National Referral Hospital today.
Initially, there was almost no equipment other than K wires to deal with fractures. As time has progressed, the open reduction, and internal fixation of fractures has become quite common. There still remains a lack of equipment and one must be quite innovative to use what is available. The lack of sterility in the entire hospital was a problem in 2003. This has steadily improved.
Over the years I watched the new hospital being built and there has been marked improvement. New operating rooms have been built which has dramatically improved the surgical capacity. The recovery room which used to be in the hallway with a little ECG monitor now looks more or less like a standard recovery room of a Canadian hospital.
Since 2016, one of the goals of Bhutanese surgeons has been to develop a total joint replacement, as there was a significant need. Prior to this I and all other volunteers would have considered it much too dangerous because of the significant potential of infection. As time has moved on, however, and it is becoming clear that this can be done in low-income countries safely the desire has increased.
On my last visit there, I spent much of my time lecturing about joint replacement indications, risks and dealing with complications. The first total joint replacement was done on December 2022.
During the COVID-19 pandemic, with the inability to travel to volunteer, I found the GCGSC and enrolled. For my assignments, I developed what I would consider an appropriate way to introduce total joints to Bhutan. I volunteered this information to the local surgeons prior to my visit in September 2022. They were already well on their way with some plans in place. I am hopeful that my six weeks spent there in constant discussions about how to proceed with total joint replacement will be of some benefit.


Could you tell us a bit more about your passion to work with volunteer-based organizations and the why behind it?
Annie: Watching my dad’s experiences around the world made me want to do something similar. I want to be able to help people around the globe, not just in my current city. I love my job – and if I can combine it with seeing the world, sign me up!
How has the GCGSC/MGSC helped you in pursuing your passion for volunteering/delivering surgical care to low-resource settings?
Doug: I do wish I’d had the opportunity to take such a program 20 years ago. Taking such a program is a benefit to anybody hoping to spend some of their practice as a volunteer. Even the preliminary courses, such as SURG 510 – Surgical Care in International Health, would make the path easier and benefit all involved in global surgery endeavours.
Annie: This program has already taught me so much. I’m fascinated by the depth and breadth of knowledge that I never knew anything about. For instance, this semester in SURG 514 – Surgical Care in Humanitarian Disaster Response, I’m learning about how the medical/surgical profession responds to disasters around the world. I always took this for granted – I never thought about the politics and strategy to set a response in motion.


